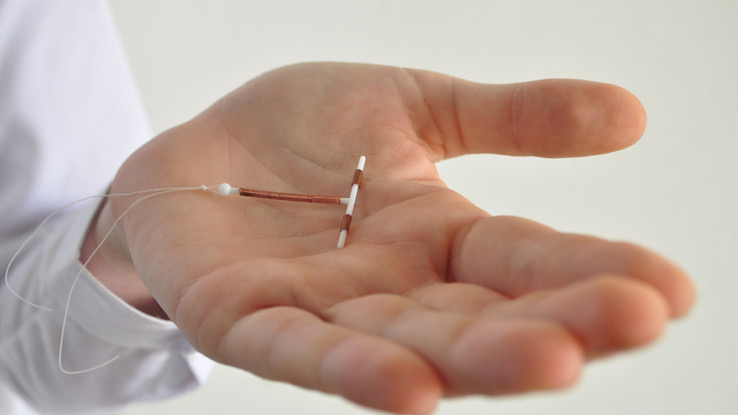
An intrauterine device (IUD) is a form of birth control. It is a small flexible plastic device in the shape of a T that a doctor puts inside the uterus (womb) to prevent pregnancy. Read on to learn more about an intrauterine device (IUD).
Types of Intrauterine Devices (IUDs)
There are two different types of IUDs available for use: copper and hormonal IUDs.
Copper IUDs
Copper IUDs are wrapped in a small length of copper wire. The copper releases ions that are toxic to sperm and eggs but are unharmful to the rest of your body, making it more difficult for the sperm to survive in the environment and for fertilization of the egg to occur. Copper IUDs are 99% effective in preventing pregnancy and last for up to 12 years.Paragard is the only brand of copper IUD that is FDA approved for use in the US.
Hormonal IUDs
Hormonal IUDs are also known as an intrauterine system or IUS. A hormone called progestin coats them and blocks the sperm from reaching the egg to fertilize it. It can also sometimes prevent the release of an egg during your monthly cycle (ovulation). Hormonal IUDs are 99% effective in preventing pregnancy and last between 3 and 7 years, depending on the brand (Skyla, Kyleena, Liletta, and Mirena).
Benefits of Intrauterine Devices (IUDs)
IUDs are an excellent option as a birth control method because they are:
- 99% effective at preventing pregnancy — Fewer than 1 out of every 100 people using an IUD will have an accidental pregnancy. An IUD is also one of the most effective ways to prevent pregnancy after having sex. You can get it within 5 days of having unprotected sex, and still be more than 99% effective.
- Long-lasting — Once you get an IUD, an IUD will work for several years. It can work for up to 7 years for hormonal IUDs and 12 years for copper IUDs.
- Reversible — A doctor or nurse can remove the device at any time, and your chances of getting pregnant will return to normal.
- Easy to use and low-maintenance — You can get an IUD at any time during your menstrual cycle, and there is minimal effort on your part. All you need to do is check the thread each month following your period to ensure the IUD is still correctly in place. Your doctor or nurse will teach you how to check this. Other than that, you can set it and forget it, which is handy if you don’t always remember with other birth control methods. It does not require partner participation, so you don’t need to interrupt sex for contraception purposes. However, it is important to know that an IUD does not protect against sexually transmitted infections (STIs). So it is recommended that you also use a condom, particularly if you are having sex with different people.
In addition, an IUD may be a better option for you than other birth control methods if you:
- Are breastfeeding — IUDs are safe to use while breastfeeding as they do not affect the quality or quantity of milk production.
- Are taking medications regularly — No medication stops an IUD from effectively preventing pregnancy. The IUD is also unlikely to interact with the effect of your other medicines.
- Have difficulty taking the hormone estrogen — IUDs do not contain estrogen. Therefore, they do not carry any risk of side effects — like acne, bloating, breast tenderness, nausea, or headaches — that some people experience when taking the combined pill or using the vaginal ring containing estrogen.
- Want lighter periods – Many users of the hormonal IUD notice decreased menstrual bleeding after a few months, sometimes leading to no vaginal bleeding at all. Others may continue to have a light regular period that is less painful than before.
Disadvantages or Possible Side Effects of Intrauterine Devices (IUDs)
Like other birth control, using an IUD as contraception has some disadvantages and side effects. The main drawback is that it does not protect against STIs, so you may still need to use condoms.
Changes to your period are the most common side effects of an IUD. This can be different for each person and depending on the type of IUD, but you may experience:
- Irregular bleeding, including spotting between periods, for the first 3-6 months. After this time, your regular bleeding pattern usually returns.
- Heavier, longer, or more painful periods for the first 3-6 months— usually with copper IUDs.
- Lighter and shorter periods, or no periods at all after 6 months— with some hormonal IUDs)
- Premenstrual syndrome (PMS)-like symptoms such as moodiness, headaches, acne, and breast tenderness— with some hormonal IUDs
The more serious but rare risks of using an IUD include:
- Rejection — it is possible that your body may push out the IUD, or it may move out of place. This is unlikely, but if it does happen, you may get pregnant. If you can no longer feel the threads or think the device has moved, see your doctor again to have it checked out.
- Pelvic infection — In the first month of having an IUD, there is a small chance of infection (around 1 in 300). Keep an eye out for any pain or tenderness in your lower abdomen, high body temperature, or an abnormal or smelly discharge. This could be a sign of infection. See your doctor immediately; they can prescribe antibiotics for treatment.
- Perforation of the uterine wall —In extremely rare cases (~0.1%), an IUD can poke through (or perforate) the wall of your cervix or uterus. If this happens, you will likely need to have the device removed surgically, which can carry additional risks.
- Ectopic pregnancy — IUDs prevent 99% of pregnancies; however, if you get pregnant with an IUD in place, it is more likely to be an ectopic pregnancy. An ectopic pregnancy is when the fertilized egg implants in one of the fallopian tubes rather than inside the womb as normal. This situation is fatal for the fetus and can be very dangerous for the mother, so you must get treatment urgently.
How To Get an Intrauterine Device (IUD)

A doctor places the IUD. As long as you are not pregnant, you can get an IUD at any time during your menstrual cycle. A copper IUD will be effective immediately after insertion. For the hormonal IUD, it will be effective against pregnancy straight away if placed within the first 7 days of your cycle. If you get an IUD at any other time, you will need to use additional contraception for at least a week to ensure you are protected.
If you think you would like to get an IUD, book an appointment with your doctor or local health clinic to discuss it. They will ask you about your medical history, including questions about your menstrual cycle, sexual activity, and any previous health problems. This is because an IUD may not be suitable for you if are pregnant or if you have:
- An STI that requires treatment
- Bleeding between periods or after sex
- Any other problems with your cervix or uterus
Intrauterine Device (IUD) Procedure
The entire appointment for placing an IUD takes around 20-30 minutes, and the actual fitting of the device should only take a few minutes from start to finish. The process is quite similar if you have ever had a pap smear (cervical screen test). Here is what you can expect:
- Your doctor or nurse will ask you to undress from the waist down and lie back on the bed with your legs bent at the knee and held slightly apart.
- They will then insert a metal or plastic device called a speculum into your vagina to hold it open.
- The IUD is then put inside an applicator tube (similar to a tampon applicator) and inserted into your cervical canal to place the IUD into your uterus carefully.
- After the doctor removes the application tube, the IUD remains in place. It has very fine strings attached to it, which hang down through the cervix.
- Your doctor or nurse will then trim the strings, so they don’t hang down too low. If you felt inside your vagina, you would be able to check that the thread is still there and the IUD is still in place.
Getting an IUD can be uncomfortable. Most people will likely feel mild cramping during the placement that lasts briefly and gets better within a few minutes. Some people may find it more painful than others. Let your doctor know if you experience any pain or discomfort — and remember you can ask them to stop.
The cost of getting an IUD depends on the type of IUD, your healthcare provider, and your insurance coverage. Check whether your health insurance plan covers birth control and up to what amount. You may also be eligible for free or low-cost IUDs through Government Programs or family planning clinics such as Planned Parenthood.
Resource Links
- “IUD” via Planned Parenthood
- “Intrauterine Device” via StatPearls
- “Intrauterine device (IUD)” via Coronavirus (COVID-19)
- “Contraception – intrauterine devices (IUD)” via Better Health Channel
- “Do the Benefits of an IUD Outweigh the Potential Side Effects?” via Cleveland Clinic





